November 22, 2016, started like any other day. It was the Tuesday before Thanksgiving, and my 12-year-old son was home for the holiday break. I was working half-days from home, juggling emails and calls while helping him clean his room. After lunch, I joined my husband at the gym for a workout, feeling energized and ready for the holiday ahead.
On our way home, we stopped at a wine shop to pick up a few bottles for Thanksgiving dinner, which we were hosting that year. Other than being a little hot and sweaty from the gym, I felt fine. But as we walked to the counter, I started to feel strange—a sensation similar to the onset of a migraine, though somehow different. I brushed it off, assuming it was just the workout catching up with me.
The feeling didn’t go away. On the short drive home, I told my husband I thought I was getting a migraine and planned to take some Advil and rest. But as we entered the house, the symptoms worsened. The right side of my face felt tingly and numb, and I started to suspect something far more serious. “I think I’m having a stroke,” I said. My husband dismissed it as dramatic and told me to rest. But as the minutes ticked by, I knew something was terribly wrong.
I Wasn’t Being Dramatic
When I tried to write my name to test my motor skills, I couldn’t grasp the pen in my right hand, let alone write. My husband called my sister, a former Neuro ICU nurse, who immediately told him to take me to the ER. By the time we arrived, I was weak, disoriented, and experiencing surreal sensations, as if I were outside my body, watching it all happen.
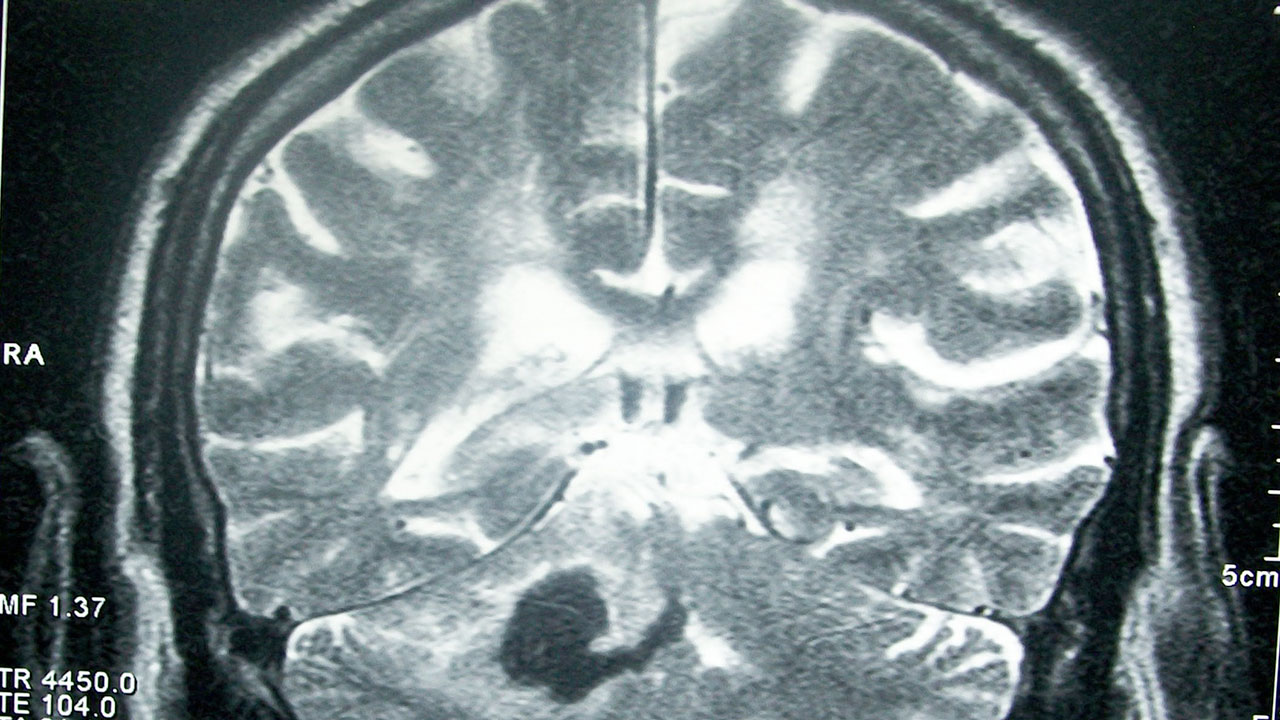
At the hospital, doctors performed a CT scan, followed by an MRI, which confirmed my suspicion: I’d suffered a stroke—a Cerebrovascular Accident, or CVA. At 38, in good health and active, I couldn’t fathom how this had happened. Tests ruled out obvious causes like clots or arterial issues, leaving me and my doctors with no clear answers. I was discharged three days later with instructions for physical and occupational therapy to recover strength and function on my right side.
In the months that followed, I focused on regaining my health. The therapy was intense, but I remained grateful that my stroke wasn’t more severe. Still, I couldn’t let go of the question: Why? Over the next four years, I saw doctor after doctor, searching for answers that never came—until a routine checkup in January 2020 finally revealed the truth.
The Answers Finally Revealed

During that visit, my general practitioner detected irregular heart palpitations, something I’d experienced sporadically for years but never thought much of. She ordered an echocardiogram, which revealed a shocking discovery: I had a congenital heart defect called Patent Foramen Ovale (PFO). It was a hole in my heart, likely present since birth, that had gone undiagnosed my entire life.
The PFO acted as a pathway for clots to bypass my lungs and travel to my brain, causing the stroke. A specialized test confirmed the hole was large enough to require closure. In a minimally invasive procedure, surgeons used a catheter to insert a closure device into my heart. The surgery was a success, and by the following day, I was home recovering.
Now, nearly eight years later, I’m fully recovered and thriving. While I’ll remain on blood thinners for the rest of my life, I feel immense gratitude for the answers I fought so hard to find—and for the chance to share my story. Not everyone gets to come out of an experience like this unscathed. If anything, I wear my “bionic heart” as a badge of honor.




